🔍 Quick Summary
- The Main Takeaway: Shifting toward more protein and fewer refined carbs can significantly stabilize blood sugar and reduce A1c, but the “quality” of your protein and fats determines your long-term heart health.
- Who This Matters For: Adults managing Type 2 diabetes or prediabetes who feel stuck on the “blood sugar roller coaster” and are looking for a sustainable way to eat without feeling constantly hungry.
- Why It’s Relevant Right Now: As we move further into a personalized health era, the “one-size-fits-all” low-fat diet is being replaced by metabolic flexibility. People are moving away from restrictive “fad” keto toward a more balanced, high-protein approach that preserves muscle mass.
High-Protein, Low-Carb Diets and Diabetes: The Part No One Explains
If you’re living with type 2 diabetes or prediabetes in the US today, you’ve probably noticed that the “diet wars” are louder than ever. One minute, you’re told to eat nothing but plants; the next, an influencer is telling you to eat steak for breakfast, lunch, and dinner. It’s exhausting. We’ve moved past the era of just counting calories, but the sheer volume of conflicting advice can make you want to throw your glucose monitor out the window.
Recently, the high-protein, low-carb (HPLC) approach has moved from niche bodybuilding forums right into the center of mainstream medical conversations. Many of our patients and peers are reporting steadier numbers and—for the first time in years—a lack of “hangry” episodes. But we also see people hitting a wall: fatigue, digestive drama, or lab results that make their doctors do a double-take.
The truth is, a high-protein, low-carb diet isn’t a magic pill, but it’s also not a dangerous fad. It’s a metabolic tool. The problem is that most explanations are either too academic or too “salesy.” We’re going to look at how this way of eating actually interacts with your biology, what the newest research says, and how you can navigate the middle ground without losing your mind.
What Actually Counts as “High-Protein, Low-Carb”?
In the world of nutrition, “low-carb” is a broad term. For some, it means staying under 20 grams of carbs a day (ketogenic territory). For most of us in the clinical and health-writing space, a sustainable high-protein, low-carb diet for diabetes usually breaks down like this:
- Protein: 25% to 35% of your daily calories.
- Carbohydrates: Under 40% of your calories, often aiming for the 100g–150g range for moderate approaches.
- Fats: The remainder of your calories, ideally coming from unsaturated sources.
This isn’t necessarily “keto.” You can still eat berries, a bit of quinoa, and plenty of leafy greens. The goal is to prioritize protein as the “anchor” of every meal so that your blood sugar doesn’t have those massive spikes and crashes that leave you feeling drained by 2 PM.
Why Protein and Carbs Play Differently with Your Blood Sugar
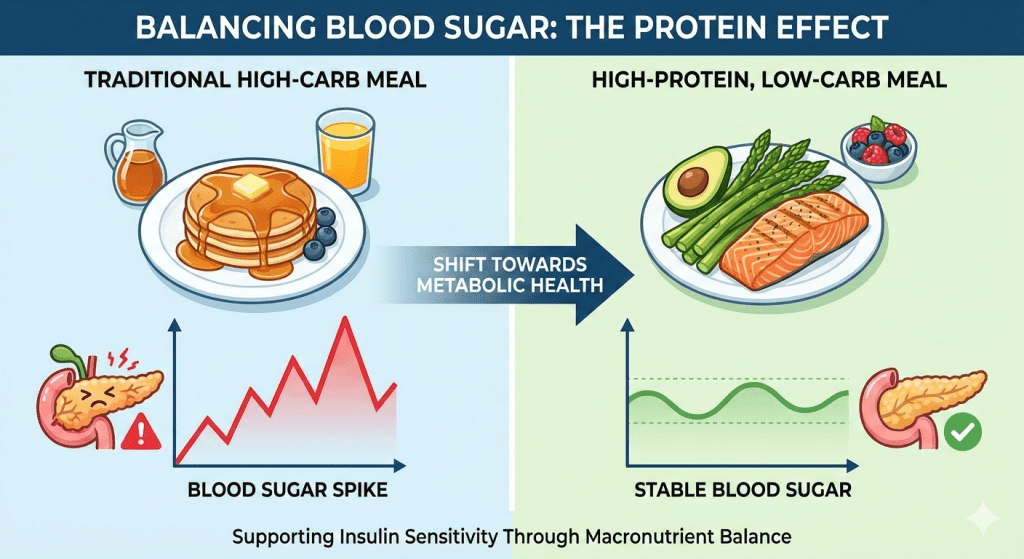
We all know that carbohydrates—especially the refined stuff like white bread or sugary lattes—break down into glucose quickly. Your body responds with an insulin spike to shove that sugar into your cells. If you have insulin resistance, that process is broken.
Protein is a different animal entirely. While it can be converted into glucose in a pinch (a process called gluconeogenesis), it happens much more slowly. More importantly, protein triggers the release of satiety hormones like PYY and GLP-1 (yes, the same ones those popular new weight-loss shots target).
When you eat a high-protein meal, you aren’t just “not eating carbs”; you are actively telling your brain that you are full. Protein also requires more energy for your body to digest—this is the “thermic effect of food.” Essentially, you burn more calories just processing a chicken breast than you do processing a donut.
What the Research Says (The Reality Check)
If we look at the latest systematic reviews, the evidence is pretty clear: reducing refined carbs while bumping up protein generally leads to better managing blood sugar levels. Short-term studies (3 to 6 months) often show impressive drops in HbA1c and fasting glucose.
However, there’s a catch. Many of these benefits are tied to weight loss. Because protein makes you feel fuller, you naturally eat less. When the weight comes off, your insulin resistance diet starts working better because your cells are less “clogged” with excess fat.
But we have to be honest—long-term data (looking 5 to 10 years out) is still a bit thin. We know it works for a year, but the “best” diet is always the one you can actually stick to without feeling like you’re in food prison.
Does This Diet Actually Fix Insulin Resistance?
This is the billion-dollar question. Insulin resistance is like a rusty lock; your “key” (insulin) is there, but it won’t turn. High-protein, low-carb diets help by:
- Reducing the Demand: By eating fewer carbs, you’re asking your pancreas to pump out less insulin. You’re giving the system a break.
- Building Muscle: Muscle is your body’s primary “glucose sink.” The more muscle you have, the more places your body has to put sugar. High-protein diets help you keep that muscle while you lose fat.
👉 Read this related guide here
However, we need to talk about cortisol. Some people go too low on carbs, which the body interprets as a stressor. This can actually raise blood sugar in the morning (the “dawn phenomenon”) because your body is pumping out stress hormones to create energy. This is why we advocate for a “smart” carb approach rather than a “no” carb approach.
The Kidney and Heart Question: Fact vs. Fiction
You’ve probably heard someone say, “All that protein is going to wreck your kidneys.” If you have healthy kidney function, the current consensus from organizations like the National Kidney Foundation is that a higher protein intake isn’t the bogeyman it was once made out to be. Your kidneys are remarkably good at filtering out the byproducts of protein metabolism.
But (and this is a big but): If you already have Chronic Kidney Disease (CKD), high protein is a genuine risk. In those cases, your kidneys are already struggling, and adding more “work” can speed up the decline. Always get your GFR (Glomerular Filtration Rate) checked before making a massive shift.
As for your heart, it all comes down to where your protein is coming from. If “high protein” means a diet of processed bacon and deli meats, your LDL cholesterol and blood pressure might head in the wrong direction. If your protein comes from a mix of lean poultry, fish, Greek yogurt, and plant sources, your heart will likely thank you.
Why Some People Feel Like Garbage at First
If you switch from a standard American diet to a high-protein, low-carb lifestyle overnight, you might feel like you have a flu. This is often called the “keto flu,” but it happens even on moderate low-carb diets.
- Dehydration: As your insulin levels drop, your kidneys dump sodium and water.
- Fiber Gap: If you cut out grains and don’t replace them with high-fiber veggies, your digestion will grind to a halt.
- The Micronutrient Miss: Cutting out fruit and certain grains can lead to low magnesium and potassium, which are crucial for heart rhythm and muscle cramps.
We recommend a “transition phase.” Instead of cutting everything at once, focus on adding protein for type 2 diabetes management first, then slowly dial back the refined sugars.
Plant Protein vs. Animal Protein: Does It Matter?
In 2026, we have more options than ever, from lab-grown meat to high-tech pea proteins. For diabetes, the source matters. Animal proteins (like eggs, whey, and lean beef) are “complete,” meaning they have all the amino acids your muscles need.
However, plant proteins (like lentils, tofu, and tempeh) come with a secret weapon: fiber. Fiber slows down the absorption of any carbs you do eat, acting like a natural brake for your blood sugar. A mix of both is usually the “sweet spot” for most people.
Quick Comparison: Protein Sources
| Protein Source | Impact on Blood Sugar | Heart Health Factor | Fiber Content |
| Salmon/Fatty Fish | Neutral | Excellent (Omega-3s) | None |
| Chicken Breast | Neutral | Good | None |
| Lentils | Low/Slow Rise | Excellent | Very High |
| Greek Yogurt | Low | Good (Probiotics) | None |
| Red Meat | Neutral | Moderate (Limit saturated fat) | None |
Is This Just Another Trend?
Low-carb eating has been around since the 1800s (look up the Banting diet if you want a history lesson). It’s not a trend; it’s a physiological strategy. What is new is our ability to track its effects in real-time with Continuous Glucose Monitors (CGMs).
We are moving away from the “diet” mentality and toward “metabolic health.” The goal isn’t just to be thin; it’s to have stable energy, clear skin, and healthy organs. If a high-protein approach helps you achieve that without feeling deprived, it’s not a trend—it’s a lifestyle.
Practical Steps: How to Start Without Overcomplicating It
If you want to try this, don’t go out and buy a 10-pound bag of protein powder just yet. Start with these three steps:
- The “Protein First” Rule: Before you touch your potatoes or rice, eat half of your protein (chicken, fish, tofu). This “primes” your digestive tract to handle the glucose better.
- Focus on Healthy Carb Sources: Swap white bread for berries, nuts, or non-starchy vegetables like broccoli and cauliflower. These provide the volume your stomach craves without the sugar spike.
- Watch the “Hidden” Carbs: Many “high-protein” bars and shakes are actually loaded with sugar alcohols or hidden starches. Read your labels like a pro.
The most important thing is to monitor. Check your levels. See how your body reacts. Everyone’s “carb threshold” is different, and in this AI-driven era of medicine, the most important data point is you.
Conclusion: The Part No One Explains
The reason people get so confused is that we treat diets like religions. The high-protein, low-carb diet isn’t “righteous”—it’s just chemistry. It works for diabetes because it tackles the root issue: glucose management and satiety.
The part no one explains is that you don’t have to be perfect. You don’t have to be in “ketosis” to see a massive improvement in your A1c. Simply shifting the balance of your plate toward protein and fiber-rich healthy carb sources can do 80% of the heavy lifting.
If you use this as a flexible framework rather than a rigid set of rules, you’re much more likely to find a version of it that you can live with for the next twenty years, not just the next twenty days.
FAQs
Can I eat too much protein if I have diabetes?
For most people, no. Your body is pretty good at telling you when you’ve had enough. However, if you have pre-existing kidney issues, you need to work closely with a doctor to find your specific “ceiling” for protein intake.
Will this diet make me tired?
You might feel a dip in energy for the first week as your body adjusts. This is usually due to a loss of electrolytes (sodium, potassium, magnesium). Adding a bit more salt to your food or eating an avocado can often fix this.
Is red meat okay for a diabetes diet?
In moderation, yes. But if you’re eating it every day, the saturated fat might negatively impact your insulin sensitivity and heart health. It’s better to rotate in fish, poultry, and plant proteins.
How many carbs should I eat a day to see a difference?
Most people see a significant improvement in blood sugar by staying under 100–150 grams of total carbs per day. Some go lower, but this range is often the most sustainable for “real life.”
Do I need to take supplements on this diet?
Not necessarily, but many people benefit from a high-quality fiber supplement or magnesium, especially if they are cutting out fortified grains and fruits.