Clinically Verified by Dr. Mian Farhan Haider, MS Clinical Nutritionist & RD
🔍 Quick Summary
- The Main Takeaway: If you’re navigating a newly diagnosed type 2 diabetes diet, early blood sugar spikes are a biological reality, not a personal failure. Your body is simply relearning how to handle fuel.
- Who Needs to Care: Anyone in their type 2 diabetes first weeks who feels frustrated or confused by seeing high numbers after eating “healthy” meals.
- Why It’s Trending Now: It’s January 2026. Between the surge in CGM (Continuous Glucose Monitor) use and the popularity of GLP-1 medications, Americans are finally seeing the “real-time” impact of food on their metabolic health.
Table of Contents
- Why Your New Diet Feels Like an Uphill Battle
- The Science of Blood Sugar Spikes After Meals
- The Usual Suspects: Foods That Spike Blood Sugar Fast
- The Oatmeal Fallacy and Other “Healthy” Triggers
- What to Eat After Diabetes Diagnosis: The 2026 Strategy
- FAQs for Your First 30 Days
<div id=”battle”></div>
Why Your New Diet Feels Like an Uphill Battle
Right out of the gate, a newly diagnosed type 2 diabetes diet can feel like the rules of engagement changed overnight. Foods you’ve eaten for decades suddenly send your glucose monitor into a frenzy. Here’s the kicker: this isn’t because you suddenly “messed up.”
Research suggests that by the time you’re diagnosed, insulin resistance has often been brewing for years. In your type 2 diabetes first weeks, your body is slower to respond to carbohydrates, especially refined ones. This “lag time” is what makes those early spikes feel so aggressive. It’s not just hype; it’s a physiological adjustment period.
<div id=”science”></div>
The Science of Blood Sugar Spikes After Meals
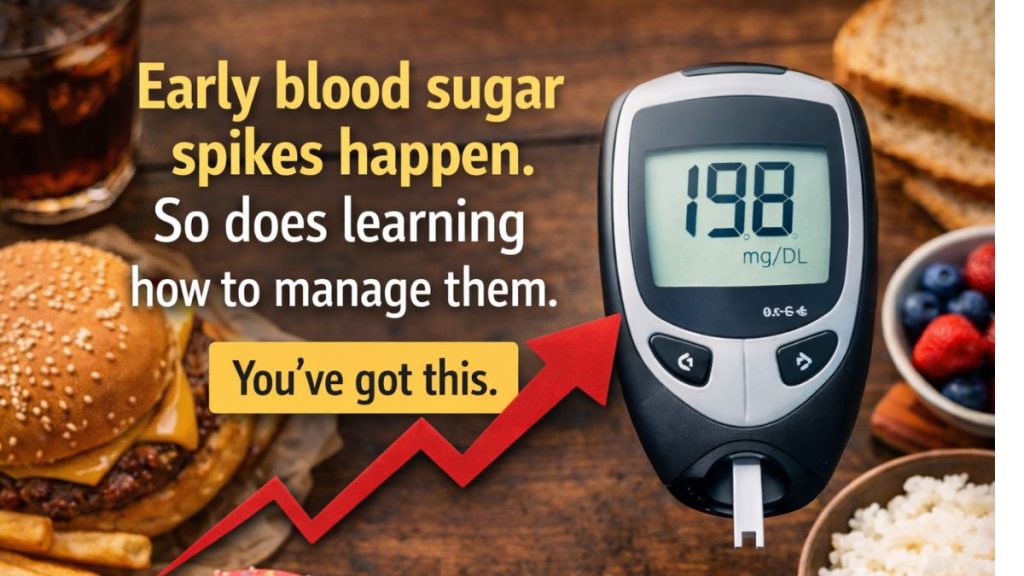
Let’s be real. A blood sugar spike isn’t a moral judgment—it’s just a measurement. Clinically, blood sugar spikes after meals refer to the rapid rise in glucose roughly one to two hours after you eat.
In a body without diabetes, insulin acts like an elite concierge, ushering sugar into your cells immediately. In early Type 2, that concierge is either understaffed or the “locks” on your cells are jammed. This causes glucose to hang out in your bloodstream much longer than it should. With more Americans using CGMs in 2026, we’re seeing these patterns with more clarity, but that visibility can be stressful if you don’t have the right context.
<div id=”suspects”></div>
The Usual Suspects: Foods That Spike Blood Sugar Fast
When you’re figuring out what to eat after diabetes diagnosis, you quickly realize that some foods are “high-velocity” triggers. These foods that spike blood sugar usually fall into four categories:
- Refined Grains: White bread, white rice, and bagels are basically glucose in a tuxedo. They digest instantly.
- Liquid Carbs: Soda is obvious, but oat milk and fruit juices are “stealth” triggers that skip the digestion line entirely.
- The “Low-Fat” Trap: Many 2026 diet snacks swap fat for starches to keep the texture, which actually makes the glycemic impact worse.
- Portion Distortion: Even “good” carbs like sweet potatoes can cause a spike if the portion is large and eaten without a protein “buffer.”
<div id=”oatmeal”></div>
The Oatmeal Fallacy and Other “Healthy” Triggers
This is where the frustration usually peaks. You swapped the donuts for a “heart-healthy” bowl of instant oatmeal, yet your numbers shot up anyway. (And no, we aren’t talking about that weird “superfood” trend you saw on social media—this is basic biology).
- Processing Matters: Steel-cut oats digest slowly, while instant oats are pre-steamed and rolled thin, hitting your system like a dessert.
- The Smoothie Myth: Blending fruit breaks down its fiber structure. Your body treats a smoothie more like a liquid than a solid meal, leading to a faster spike.
- Fruit Sequencing: Eating a banana on an empty stomach vs. eating it after a high-protein breakfast results in two completely different glucose curves.
Expert Insight: If you’re currently on a medication path involving GLP-1s, your nutritional focus should be even more targeted. Check out our GLP-1 Diet Plan & Nutrition Guide for specific tips on maintaining muscle while managing glucose.
<div id=”strategy”></div>
What to Eat After Diabetes Diagnosis: The 2026 Strategy
So, what to eat after diabetes diagnosis when everything feels like a minefield? In 2026, the consensus has shifted from “No Carbs” to “Smart Sequencing.”
The heavy lifting is done by your meal order. Research from Harvard Health and other major institutions suggests that eating fiber (veggies) and protein (chicken, eggs, tofu) before you touch a carb can blunt a spike by up to 40%. It’s a total game-changer. By the time the carbs hit your system, the protein and fiber have already slowed down the “emptying” of your stomach.
<div id=”faqs”></div>
FAQs: Navigating Your First 30 Days
Why does my blood sugar spike more right after diagnosis? Your insulin response is likely at its weakest right now, and “glucose toxicity” can temporarily make your cells even more resistant to insulin. As you stabilize, this often improves.
Are blood sugar spikes after meals always dangerous? A single spike isn’t a verdict. Doctors look at long-term trends (like your A1c). Think of a spike as a data point that helps you tweak your newly diagnosed type 2 diabetes diet.
Can I ever eat fruit again? Yes. Stick to high-fiber options like berries and always pair them with a fat or protein (like almonds or Greek yogurt) to slow down the sugar hit.
How do I find out which foods spike me personally? Test your glucose before a meal and then 1–2 hours after. If the jump is more than 50 points, that food might need a “protein pair” or a smaller portion.
Should I go “Zero Carb” in my first weeks? The CDC and most dietitians recommend sustainable, individualized plans over extreme restriction. “Zero Carb” is rarely a long-term win.

