Clinically Verified by Dr. Mian Farhan Haider, MS Clinical Nutritionist & RD
🔍 Quick Summary: GLP-1 medications like semaglutide and tirzepatide have revolutionized weight management, but they’ve created a new paradox: how do you nourish a body that doesn’t want to eat? By January 2026, the focus has shifted from simple weight loss to muscle preservation and metabolic health. The strategy isn’t eating less—it’s eating smarter. This guide breaks down the “GLP-1 diet plan” for the real world: prioritizing protein density, hacking digestion to avoid nausea, and stabilizing blood sugar without the bulk.
The Main Takeaway
Appetite suppression is a feature, not a hall pass to skip nutrition. The goal is to pack maximum nutrient density into minimum volume (think “high-performance fuel,” not “diet food”).
Who Needs to Care
Anyone currently taking GLP-1 receptor agonists (Wegovy, Zepbound, Ozempic, Mounjaro) or those supporting them.
Why It’s Trending Now (2026 Context)
We’ve moved past the initial hype cycle. Now, the data is showing that long-term users are struggling with sarcopenia (muscle loss) and nutrient deficiencies because they simply can’t stomach the food they need. The 2026 conversation is all about “quality over quantity.”
The New Rules of Engagement: Eating on GLP-1s
Let’s be real for a second. If you’re on a GLP-1 medication, your relationship with food has probably done a complete 180. The “food noise” that used to scream at you for a 3 PM snack? Gone. But in its place is a new, quieter problem that’s arguably trickier to solve: malnutrition by accident.
Right out of the gate, we need to address the elephant in the room. Drugs like semaglutide and tirzepatide slow down your gastric emptying (basically, your stomach hits the brakes). This makes you feel full faster and longer. While that’s a massive win for the scale, it’s a logistical nightmare for getting enough protein and fiber.
The buzzword floating around clinics and Reddit threads right now is “GLP-1 Friendly.” But what does that actually mean? It’s not just a trendy marketing label on a protein bar. It’s a physiological necessity. When your stomach capacity drops by half (or more), every single bite has to pull its weight.
What “GLP-1 Friendly” Actually Looks Like
Despite what you might see on social media, there is no official “Ozempic Diet.” (And no, we aren’t talking about that weird cottage cheese trend you saw last week). At the end of the day, a GLP-1 friendly meal plan is just clinical nutrition adapted for a micro-appetite.
If you’re building a plate in 2026, it needs to check four specific boxes:
- Density is King: You don’t have the luxury of “empty calories” anymore. If you can only eat 10 bites, 8 of them need to be nutrient-dense.
- Volume Control: Meals need to be compact. Big salads are great in theory, but the sheer volume can trigger early satiety and leave you bloating for hours.
- The “Vibe-Check” for Digestion: Foods need to be gentle. Anything too greasy, spicy, or fibrous can turn a good day into a nausea nightmare.
- Glucose Guardrails: Even though the meds help with blood sugar, you still want to avoid rapid spikes to keep your energy stable.
The Muscle Math: Why Protein is Non-Negotiable
Here’s the kicker: eating less doesn’t automatically mean you’re getting healthier. The most significant risk we’re seeing in long-term GLP-1 users is the loss of lean muscle mass.
When you lose weight rapidly, your body will happily burn muscle for fuel if you aren’t feeding it enough protein. This matters for your metabolism, your strength, and how you look and feel. But because these drugs mute your hunger cues, you might not feel the urge to eat that chicken breast or tofu block.
The heavy lifting here involves hitting a target of roughly 1.0 to 1.2 grams of protein per kilogram of body weight. That’s a lot of protein when you aren’t hungry.
How to Hack Your Protein Intake

You can’t just sit down to a 12-ounce steak anymore. It won’t happen. You have to be strategic:
- Protein First: Eat the protein on your plate before you touch the veggies or carbs. If you get full, at least you banked the amino acids.
- Liquid Gold: If chewing feels like a chore (a common side effect), lean into bone broths, high-quality protein shakes, or yogurt drinks.
- The “Graze” Method: Instead of three square meals, aim for five “mini-fuelings.” A hard-boiled egg here, a slice of turkey there. It keeps the nutrients flowing without overwhelming your stomach.
Navigating the “Ick”: Nausea and Digestion
We can’t talk about these meds without addressing the nausea. It’s the most common complaint, especially when you’re titrating up a dose.
The culprit is usually food sitting in your stomach too long. If you eat a high-fat meal (like a burger) or a high-fiber meal (like a massive bowl of raw kale), it sits there like a brick.
The Fix:
- Go Soft: Cook your veggies until they are soft. Bake or steam your proteins.
- Temperature Matters: Sometimes, cold or room-temperature foods smell less intense and are easier to tolerate than hot, aromatic meals.
- Hydrate, Don’t Flood: Sip water throughout the day, but don’t chug a pint with your meal, or you’ll feel painfully full.
The Fiber Balance: Avoiding the Backup
Let’s be honest—constipation is a real issue on these meds. The instinct is to load up on fiber supplements, but that can backfire if you aren’t drinking enough water, turning a blockage into a blockade.
The strategy is “low and slow.” Incorporate soluble fibers like oats, chia seeds, and berries. These absorb water and move things along more gently than roughage like raw bran or broccoli stems.
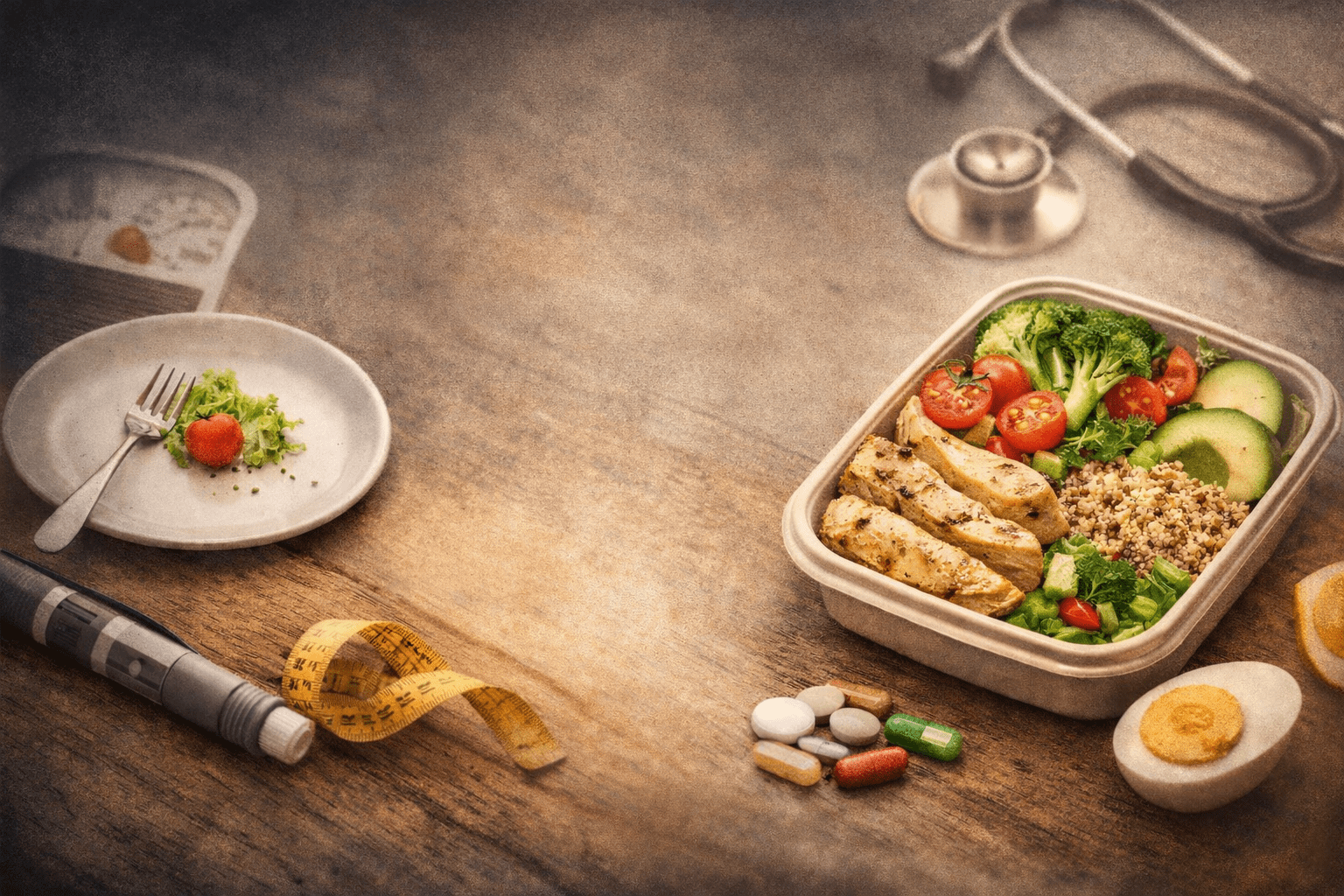
Building Your Plate: The 2026 Blueprint
You don’t need a degree in nutrition to get this right. Visualize your plate (or bowl, since bowls are often easier psychologically) like this:
- The Anchor (Protein): 3-4 oz of salmon, chicken, tofu, or Greek yogurt.
- The Support (Veggie): A small scoop of roasted carrots, spinach, or green beans.
- The Fuel (Fiber Carb): A few tablespoons of quinoa, lentils, or berries.
- The Finisher (Healthy Fat): A slice of avocado or a drizzle of olive oil.
It’s not exciting, but it works. It keeps your blood sugar stable, protects your muscle, and minimizes the risk of spending the evening feeling gross.
The Bottom Line
GLP-1 medications are a massive tool in the toolbox, but they don’t do the work for you—they just change the work you have to do. The game in 2026 isn’t about restriction; it’s about intentionality.
It’s about looking at a smaller plate and ensuring it has everything your body needs to thrive, not just survive. If you’re checking the boxes on protein and hydration while listening to your body’s new signals, you’re already winning.
For reference, check these sites:
- CDC: Healthy Weight, Nutrition, and Physical Activity
https://www.cdc.gov/healthyweight/index.html - Mayo Clinic: GLP-1 Agonists & Weight Loss
https://www.mayoclinic.org/diseases-conditions/type-2-diabetes/expert-answers/byetta/faq-20057955 - Cleveland Clinic: GLP-1 Agonists – What To Eat & Avoid
https://my.clevelandclinic.org/health/treatments/13901-glp-1-agonists
💡 PRO-TIP: THE PROTEIN SHORTCUT Finding the right protein sources that don’t break the bank is half the battle when you’re on a GLP-1. If you’re looking to stock up on the best high-density options for your pantry, check out our curated guide to the Best Costco Protein for Diabetes. It’s the ultimate cheat sheet for hitting your protein goals without the guesswork.